Endoscopic Retrograde Cholangiopancreatography ERCP Youngstown
ERCP Youngstown
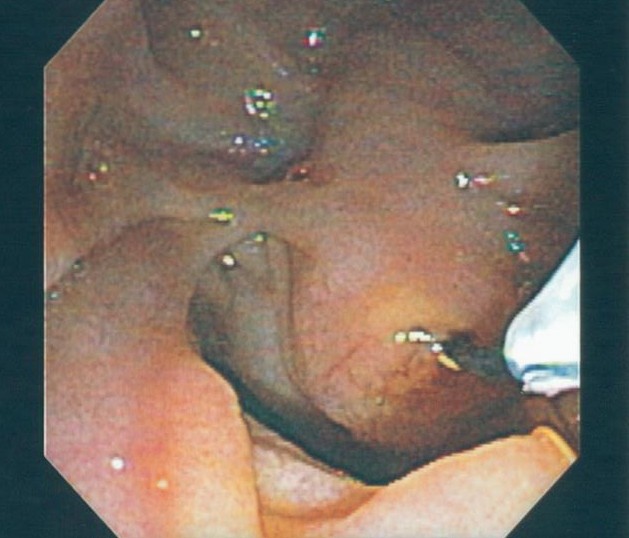
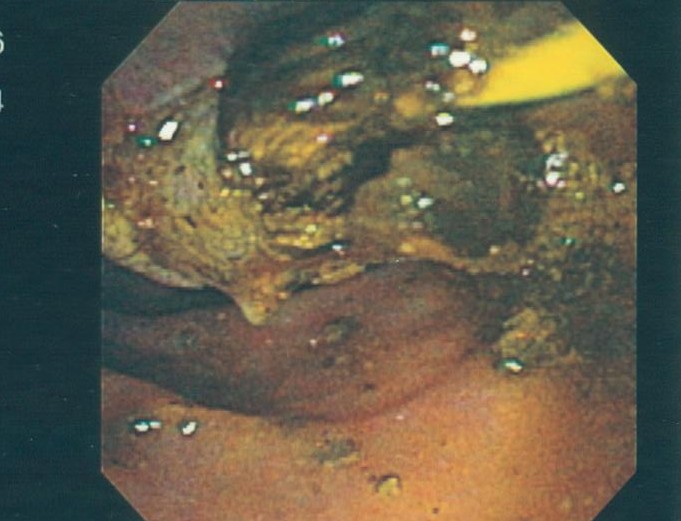
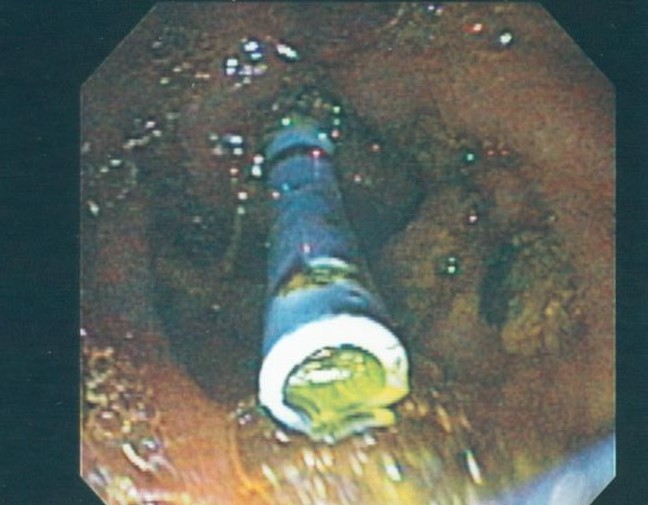
An ERCP is a specialized, endoscopic procedure used to evaluate and treat disorders in the liver (bile) and pancreatic ducts. A flexible camera the size of your index finger is placed into the mouth and passed down through the stomach into the first part of the small intestine (duodenum). A tiny, pin-hole opening (ampulla) leads to the bile and pancreatic ducts is cannulated with a wire. Dye is injected into the ducts, and xrays are taken. Specialized instruments may be used in the ducts to dilate, biopsy, stent, and do other procedures.
Why is an ERCP performed?
An ERCP is performed to evaluate and treat suspected disorders of the liver and pancreas. Blockage of the liver ducts may be due to disorders such a gallstones and tumors. Strictures in the pancreas may cause recurrent pancreatis. Patients with chronic abdominal pain or post-cholecystectomy pain may actually have a disorder where the muscle around the ampulla is tight or spastic leading to back-pressure in the bile duct (sphincter of Oddi dysfunction). Symptoms from sphincter of Oddi dysfunction often mimic gallbladder symptoms (abdominal pain, nausea, and/or bloating).
Complications from an ERCP
An ERCP is a minimally invasive technique that is perform entirely endoscopically (through the mouth without making incisions outside the body). The complication rate is therefore significantly less than open procedures performed before ERCP was available. Even though it is relatively safe, complication do exist for the procedure. The most common complication is pancreatitis due to irritation of the pancreatic duct that shares the same opening as the bile duct.
Pancreatits occurs about 8% of the time post-ERCP but occurs more frequently in certain circumstances (patients with chronic pancreatitis or those requiring pancreatic procedures, difficult cannulation, and those with suspected sphincter of Oddi dysfunction). Pancreaitis is treated with IV fluids and bowel rest. It usually resolves within a couple of days if it occurs. Studies have also shown that placing a temporary pancreatic stent decreases pancreatitis and should be placed in higher-risk patients. Other risks are <1% and include bleeding, infection, and perforation.